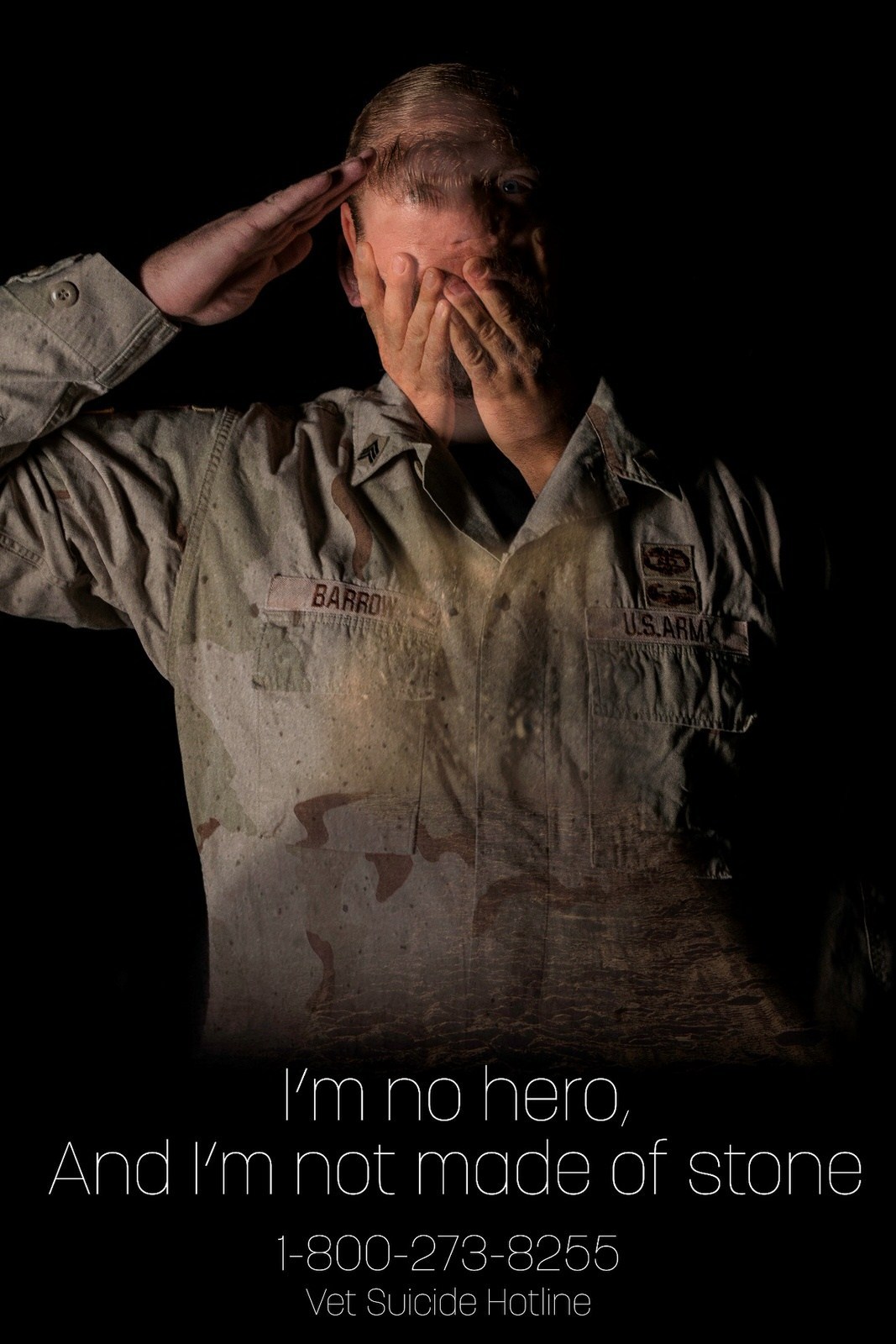
Mental Health Awareness: Military and First Responders
First Responders and Military personnel are routinely exposed to traumatic events in the course of their duties. They often must make life and death decisions in a split-second, with razor-thin margins for error. As such, these men and women are at increased risk for behavioral health conditions and long-term problems from traumatic stress.
The National Alliance on Mental Illness lists the following conditions as concerns for those serving in the military.
It is estimated that 30% of first responders develop behavioral health conditions during their time of service. The below mental health concerns also apply for first responders.
Mental Health Concerns
- Posttraumatic Stress Disorder (PTSD). Traumatic events, such as military combat, assault, disasters, or sexual assault can have long-lasting negative effects such as trouble sleeping, anger, nightmares, being jumpy, and alcohol and drug abuse. When these troubles don’t go away, it could be PTSD. The 2014 JAMA Psychiatry study found the rate of PTSD to be 15 times higher than civilians.
According to an article from the Harvard Review of Psychiatry, “over the past two decades, a growing body of research has yielded prevalent estimates for the development of PTSD in first responders following work-related exposure to traumatic events. This data was derived mostly from small-scale, retrospective studies utilizing self-report measures, rather than from diagnostic clinical interviews. As such, results must be interpreted judiciously. Nevertheless, cumulative range estimates can serve as potentially reliable indicators of PTSD prevalence. Studies show that LEOs develop PTSD at rates ranging from 6% to 32%, EMT/paramedics at rates ranging from 9% to 22%, and Firefighters at rates ranging from 17% to 32%. By contrast, approximately 7% to 12% of adults in the United States will develop PTSD at some point in their lifetimes.”
- Depression. More than just experiencing sadness, depression doesn’t mean you are weak, nor is it something that you can simply “just get over.” Depression interferes with daily life and normal functioning and may require treatment. The 2014 JAMA Psychiatry study found the rate of depression to be five times higher than civilians.
- Traumatic Brain Injury (TBI). A traumatic brain injury is usually the result of a significant blow to the head or body. Symptoms can include headaches, fatigue or drowsiness, memory problems, and mood changes and mood swings.
In addition to the mental health concerns NAMI provides, Anxiety is also a concern first responders and military service members are at risk for.
- Anxiety. Anxiety symptoms that last for six months or more generally qualify for a diagnosis of generalized anxiety disorder (GAD), social anxiety disorder, panic disorder, obsessive-compulsive disorder (OCD), or phobia. The specific symptoms will vary depending upon the disorder but may include intense fears of specific places or things, obsessive thoughts that are intrusive, disrupted sleeping and eating patterns, substance abuse, and more.
Secondary Trauma
Exposure to the traumatic experiences of others —known as secondary, or vicarious trauma—is an inevitable challenge for first responders. 911 Telecommunicators are especially prone to secondary trauma.
Coping with the effects of others’ trauma can be draining and can have lasting negative effects. Self-care, peer support, and counseling are some of the ways to mitigate the impact of secondary trauma.
Addiction
There is no one reason that people drink or use drugs. Numerous risk factors can make substance abuse more likely. When a person turns to alcohol or drugs for self-medicating purposes, they are more likely to become dependent upon that substance than an individual that is a recreational user.
Military
An American Addiction Centers article states that “research on military conflicts in Iraq and Afghanistan have shown that both deployments and exposure to combat are correlated with increased alcohol intake, heavy/binge drinking, and other alcohol-related problems. In 2015, 30% of active-duty service members were binge drinkers. Just over one-third either engaged in hazardous drinking behaviors or met criteria for alcohol use disorder (AUD).”
“In 2015, less than 1 percent of active-duty military service personnel across all branches reported any illicit drug use,” states the American Addiction Centers.
However, the AAC article continued, “rates of prescription drug abuse are similar to those of the general population. In just 8 years between 2001 and 2009, the number of painkiller prescriptions written by military doctors quadrupled.”
First Responders
Adverse mental health conditions can lead vulnerable first responders to turn to drugs and/or alcohol to cope with and mask their pain. The continued stigma surrounding mental health may also make first responders more resistant to treatment than the general population.
According to Mission Harbor Behavioral Health, “alcohol is the most commonly abused substance of first responders, [especially those] with PTSD. There are many different reasons for this, and chief among them is that alcohol and drinking are socializing events. First responders who share the witnessing of traumatic events will often drink together as a form of stress relief and a way to bond over the trauma.”
“A recent study from the University of Arizona found that alcohol abuse and addiction rates increased the longer the study participants worked as police officers,” continued Mission Harbor Behavioral Health. “Rookies who join the force and report 0% will experience an accumulation of job stress. After two years, 27% of rookies go on to develop an alcohol use disorder. After four years on the force, that number increases to 36%. The study also found that alcohol use is a deeply ingrained part of police force culture.”
Mission Harbor Behavioral Health states that “the U.S. Firefighters Association estimates that 10% of all firefighters abuse drugs. 29% of firefighters abuse alcohol. Compared to statistics in 2013 which indicated that 6.6% of the general population abused alcohol.”
The American Addiction Centers indicated that “drug abuse is much higher among paramedics and EMTs compared to other emergency responder professions. The limited research has not yet come to conclusions as to why, but it is believed to be a combination of factors including easy access to potent and addictive prescription medications and high-stress exposure levels.”
Treatment
Treatment for first responders and military personnel is the same as it is for the general population. However, many agencies have in-house or regional resources for their members to utilize as they need. These resources are specialized and often have retired law enforcement, firefighters, EMTs, or military members available.
Immediate Help:
If you or someone you know is in crisis, know that someone is always available. No one fights alone.
The National Suicide Prevention Lifeline – 1-800-273-8255.
The National Suicide Prevention Lifeline (ESP) –1-888-628-9454
The National Suicide Prevention Lifeline (Deaf & Hard of Hearing Options) – 1-800-799-4889
The National Suicide Prevention Lifeline Chat – https://suicidepreventionlifeline.org/chat/
Crisis Text Line – Text HOME to 741741 in the US
National Domestic Abuse Hotline:1-800-799-7233
National Domestic Abuse Hotline (TTY): 1-800-787-3224
The Veterans Crisis Line – 1-800-273-8255, Press 1.
Reddit Suicide support: https://www.reddit.com/r/SuicideWatch/
Suicide.org list of local helplines for all 50 states: http://www.suicide.org/suicide-hotlines.html
Suicide survivor support groups: http://tinyurl.com/m47k5en
BY ELIZABETH MILLER